Previous : Doubling Down on Hormone Therapy
Next : Let food be they medicine …
#prostatecancer #cancer #prostatitis #psa #prostate #urology #oncology #drawnandcoded #iwillbeatthis #comics #radiology #mri #radiologist #researchstudy #clincialstudy
Previous : Doubling Down on Hormone Therapy
Next : Let food be they medicine …
#prostatecancer #cancer #prostatitis #psa #prostate #urology #oncology #drawnandcoded #iwillbeatthis #comics #radiology #mri #radiologist #researchstudy #clincialstudy

Sexy, right? Amazon sells a model with a larger pill capacity but this one screams “minimalist and sleek” to me. Why a pill box? Because my medications keep increasing in number and complexity. As food can have a big effect on how a medication is absorbed in your body, it’s important to take some medications based around meals. The most logical way to do this is to organize pills by mealtime in cute, colorful, OCD-inducing plastic boxes.
This week is Thanksgiving.
Up until this year I’ve been the underdog in these conversations. However, this year is different! This year I get to slap my new pill box down and insert myself into the conversation with gusto! Maybe I’ll even raise the ante a bit and sneak a couple of placebo pills in as well!
Honestly, it’s a little disconcerting. In less than 6 months I’ve gone from no medications at all to enough to require, well, a pill organizer. My friend, Missy pointed out that it’s not forever. Retired from the Navy she used deployments as an analogy. She told me, “Deployments take two years. They suck, but in the end you get to come home and return to your normal life.” Coincidentally, my friend Pat who also has prostate cancer just ended his “deployment” and is doing great after concluding two years of treatments.
So, what goes into my pillbox?
The latest medication is Zytiga. Zytiga is used to treat aggressive prostate cancer, like mine. It along with Prednisone and the Firmagon shots that I started last week, complete the hormone therapy cocktail prescribed to me by my oncologist, Dr. Stewart. Dr. Stewart told me that Zytiga stops my adrenal glands from producing testosterone. If you remember from my prior post, testosterone feeds prostate cancer. Without testosterone the cancer should stop metastasizing and shrink. Zytiga is just another way of crimping the fuel line. One of the side effects of Zytiga is that it lowers the amount of cortisol produced by the adrenal glands. Cortisol, known as the “stress hormone” helps regulate blood pressure, metabolism, and stress levels. Sounds important, right? The Prednisone is a synthetic cortisol to replace what is lost when taking Zytiga. I also need to take vitamin supplements such as calcium to maintain bone density and prevent muscle loss. Zytiga can also cause high blood pressure and liver problems. While taking it I will need to monitor my blood pressure daily and have blood drawn every two weeks to check my liver function.
Yes, the zeros are in the right place. That’s roughly $160 per pill. I take two pills per night. My prostate cancer cells apparently have very very exquisite tastes. In retrospect maybe I should have bought a pill box with a padlock…
I wish I could peg the blame solely on some greedy pharmaceutical executive somewhere pricing these things. In reality, I know that the truth is a lot more complicated than that. Zytiga, being approved in 2011, is a relatively new medication. Newer medications can take up to a decade and well over a billion dollars to get approved. Of all potential candidates only 10% are ever approved by the Food and Drug Administration ( FDA ) for the market. That’s a lot of money and a lot of risk.
Thankfully, my health insurance helps a lot with the costs. I now understand why insurance rates increase annually as treatments like this skyrocket in price. No, it’s not okay and it’s definitely not sustainable but I’m at a loss how to fix the problem.
Last night after I choked down my jagged little pills Jodie showed me a study that she had found with an innovative solution for cutting costs. Earlier I mentioned how some medications are absorbed differently based upon what they are taken with. Zytiga, for this reason, is taken on an empty stomach. The study found that if Zytiga were instead taken with food, the dosage could be halved and have the same overall effect. At $160 per pill the study estimated that the savings per patient were in the hundreds of thousands of dollars. Although the study hasn’t been clinically approved it is refreshing and a step in the right direction.
Take care. Stay healthy. Live life. Have a Happy Thanksgiving!
-Scott
Previous : Manopause
Next : A Research Study

#prostatecancer #cancer #prostatitis #psa #prostate #urology #oncology #drawnandcoded #iwillbeatthis

“Hormone therapy generally makes everything shrink”, the radiation oncologist told me.
“Like, everything?”,I asked.
“Yes.”, she replied.
( Cough, Cough )
“Everything everything?”
“Yes, it’s a potential side effect.”
“Can I, uh, quote you on that?”, I replied.
“Sure!”, she said with a smile.
And then she explained to me how shrinkage was a good thing – at least for future treatments. Smaller tumors mean less invasive surgery. Smaller tumors also mean less radiation when undergoing radiation treatment. You’ve heard it here first.
She explained that hormone therapy also starves “free floating” cancer cells that have broken away from the main tumor. By starving and killing these vagrant cells the hope is to stave off metastasis to other organs.
If cancer cells break off from the main tumor and spread somewhere else, the new tumor is still the same type of cancer. Prostate cancer that has spread to the bones is still very much prostate cancer and as such can be treated with similar therapies, such as hormone therapy. Cancer that originated in the bones is a different type of cancer altogether and as such must be treated differently.
The upside of all this, at least for prostate cancer, is that the PSA score is a systemic indicator of prostate cancer in the entire body – not just within the prostate. If the prostate is removed for example, and the PSA score keeps going up, chances are good that the prostate cancer has found a new home elsewhere. That’s the bad news. The good news is that the same arsenal of treatments are effective against it no matter where it is. Well, as long as the treatments can reach it.
After being told of the side effects and reading one too many reviews online I thought I was in for pure hormonal hell. So far my fears have been exaggerated.
I now have large painful bumps to the left and right of my belly button. Sneezing of course, hurts. So does sitting up from a prone position. When laying down I’ve opted to flop around like a beached seal instead of twisting. I wake up a lot, too, but I seem to fall back asleep easily enough. I can only assume that this is a result of the other side effects of the medication. The worst pain so far? The removal of the band-aids that were covering the injection site from my unshorn belly.
Everything takes just a little more effort. I’m more tired, a little spacey, and forgetful. I was told to lift weights to counteract the muscle mass and bone density that is lost as a result of the hormone therapy. I’ve managed, but I get winded faster and everything feels just a little heavier. I’m lucky in that I have a sedentary job where the heaviest thing I need to lift is a computer mouse. If I were moving furniture however, I’m pretty sure I’d be well, screwed.
This is what I was worried about most. Just thinking about anxiety makes me anxious. If you remember the 80’s movie Beetlejuice, when the titular characters’ name is said aloud too many times he jumps out and terrorizes everyone. Well, anxiety for me is kind of like that. I have an entire bandoleer of Ativan at the ready if necessary, but so far I haven’t had to use it. Staying in the moment has helped the most. As there is no clear path for my treatment yet, worrying about it is probably the worst thing I can do.
They’re not bad and they are rare, but they happen. I can best describe the sensation by flip-flopping the typical advice given to someone for public speaking: Picture yourself naked on stage talking to a large clothed audience. That, to me, is what a hot flash feels like.
A couple of days after my first treatment our neighbors invited us on a hike. While we were getting ready my oldest daughter, Ashley shoved one of those battery-powered handheld fans into my hands. This one in particular even had a water reservoir.
“Here, dad!”, she said excitedly.
“Uh, thanks… um, why?”, I replied.
“In case you have hot flashes on our hike!”, she said proudly.
So, yes. My daughters have my back. It’s reassuring to know that when menopause hits the Vandervort household someday that I can take at least some credit in grooming my girls to take care of their mom, too.
Last but not least, I bought Jodie and the girls necklaces to wear to mark the start of my cancer treatment. The necklaces are simple silver chains, each adorned with three heart pendants. One heart for each girl. To me the necklaces are a symbol of solidarity. It seemed an appropriate gift for the three people who are going to be on the front lines with me throughout this fight.

Take care. Stay healthy. Live life.
-Scott
Previous : Let the games begin…
Next : Doubling down on hormone therapy

#prostatecancer #cancer #prostatitis #psa #prostate #urology #oncology #drawnandcoded #iwillbeatthis

Today, Jodie and I drove to UCSD for my first hormone therapy treatment. As I mentioned in my previous post I was to be given Degarelix, more comically known as “Firmagon”, to reduce my testosterone levels. My nurse reiterated the side effects before describing how the medication would be administered.
“The shots will be given using a really small needle…”, my nurse said.
“Wait…shots? Plural?”, I responded.
“…to your belly…”, she resumed.
“Uh….”, I replied.
“…and it requires a loading dose of two shots. One on each side…”, she continued.
“…”
“…and together the shots will contain roughly three times the serum as a normal dose.”
“You’re not really selling this that well, you know.”, I told her.
“I have some ice packs for you to use afterwards. You will likely have some pain at the injection site for a couple days on up to a week. There will also be some swelling and redness.”, she responded.
“Swelling? Can you at least distribute the shots to look like I have abs?”, I requested.
At this point Jodie offered some Tylenol capsules which she had brought along for the occasion. The nurse quickly had me take them before preparing the shots.
“If I scream like a little girl don’t take it personally. You look like a nice person.”, I told the nurse before laying down on my back and pulling back my shirt.
“Oh, you don’t have much of belly. That’s going to make this a little more tricky…”, the nurse said before starting the first injection.
Fortunately, Jodie was able to capture the entire procedure on film for posterity. It went down something like this …


Okay, I might be exaggerating a little.
The administering of the shots didn’t hurt much more than a flu shot. My nurse did an incredible job. The jury is still out on residual pain but I’ll be sure to post on that in the future if it is an issue.
A couple of band-aids later Jodie and I headed back to the parking garage. As I started backing out of the parking spot Jodie told me, “I have a special song for the occasion!”
“Uh, okay”, I said smiling.
She then started playing Stone Temple Pilots, “Creep” which ironically, was one of my favorite songs from high school. I didn’t quite understand the relevance until the chorus. When it played we sang aloud and had a good laugh. My wife has an odd sense of humor as I do…
Forward yesterday makes me wanna stay
What they said was real makes me wanna steal
Living under house guess I’m living I’m a mouse
All’s I gots is time got no meaning just a rhyme
Take time with a wounded hand ’cause it likes to heal
Take time with a wounded hand ’cause I like to steal
Take time with a wounded hand ’cause it likes to heal,
I like to steal
I’m half the man I used to be (this feeling as the dawn it fades to gray)
Well, I’m half the man I used to be (this feeling as the dawn it fades to gray)
Well, I’m half the man I used to be (this feeling as the dawn it fades to gray)
Well, I’m half the man I used to be
Half the man I used to be
…okay, maybe not exactly half the man.
Jodie pointed out later that the Firmagon marketing material advertises an 88% drop in testosterone on the first day. “So, you’re effectively 12% the man you used to be!”, she said smiling at me.
“Thanks, honey.”
Take care. Stay healthy. Live life.
– Scott
Previous : Renewed Interest
Next : Manopause
#prostatecancer #cancer #prostatitis #psa #prostate #urology #oncology #drawnandcoded #iwillbeatthis

Previous : Drug Interactions
Next : Let the Games Begin

#prostatecancer #cancer #prostatitis #psa #prostate #urology #oncology #drawnandcoded #iwillbeatthis #drawnandcoded #scottsjewelscomic #comic #sketchbook

Before a biopsy diagnosed me with prostate cancer my doctors all thought that I had prostatitis, a painful inflammation of the prostate. The symptoms of prostatitis are very similar to a urinary tract infection – frequent urination, burning while urinating, interrupted urine stream, pelvic pain, and so on. The big difference is that while a urinary tract infection can generally be cured with antibiotics, the majority of cases of prostatitis cannot. Chronic prostatitis, or prostatitis that lasts longer than three months is sometimes called Chronic Pelvic Pain Syndrome ( CPPS ).
My doctor prescribed 60-days worth of antibiotics including Doxycycline, Ciprofloaxcin, Bactrim, and Clindamycin. None of these worked. Next, he prescribed me physical therapy to help relieve tension. This along with reading books on self-help, psychosomatic pain, and CPPS helped, but my anxiety still worsened. It got to the point where I was anxious about being anxious – a vicious circle. Anxiety, I realized caused me to tense up which resulted in additional pain which ( you guessed it ) caused me to get even more anxious. Inflamed prostates, like porcupines, don’t like being “squeezed”. Before long I was having trouble getting out of bed and going outside without having an anxiety attack.
So, I saw a psychiatrist and was prescribed Lexapro, an anxiety medication belonging to a group of medications known as SSRIs, or “Selective serotonin reuptake inhibitors”. An SSRI increases the serotonin uptake in your brain. Serotonin is a chemical that improves well being and happiness. SSRIs need to be taken for a few weeks before they start working. During that time your symptoms can unfortunately, worsen. Conversely, when you stop taking an SSRI you risk going through withdrawal symptoms – especially if you quit cold turkey.
So, by now you’re probably wondering where the heck I am going with this.
Well, as it turns out SSRIs don’t play well with hormone therapy drugs such as Firmagon. When used together they have what is known as a ”drug interaction”. Unlike the combination of foods like say, peanut butter and jelly, combining drugs isn’t always a good thing. Combining Lexapro and Firmagon for example, can cause a potentially serious irregular heartbeat.
Yeah, let’s just avoid that one, m’kay.
As cancer treatment trumps anxiety the Lexapro sadly, must go. I talked to my pharmacist about how to go about weaning myself off Lexapro. She said that the conventional method is to halve the dosage the first week and then to skip days with the halved dosage the next week. She also warned that stopping Lexapro, in addition to removing all of the stops on whatever anxiety it was keeping in check in the first place, has its own list of side effects as well : anxiety, depression, mood swings and so on. She did not recommend abruptly stopping.
So, what’s the good news? Well, I’m reaching here but to me it seems like the side effects of hormone therapy and Lexapro withdrawal are well, somewhat complementary. I mean what goes better with mood swings and depression than hot flashes, right? Fortunately, my doctor suggested that there are alternative anxiety medications that I can take. At my next appointment I will be sure to ask him.
Tonight I am going to start halving my Lexapro tablets. If my wife, Jodie has her way with the insurance company I will likely start hormone therapy within the next day or two as well. The next couple of weeks should be entertaining to say the least. Wish me ( and everyone in my immediate vicinity ) luck…
Take care. Stay healthy. Live life.
-Scott
Previous : Treatment Options
Next : Renewed Interest

#prostatecancer #cancer #prostatitis #psa #prostate #urology #oncology #drawnandcoded #iwillbeatthis

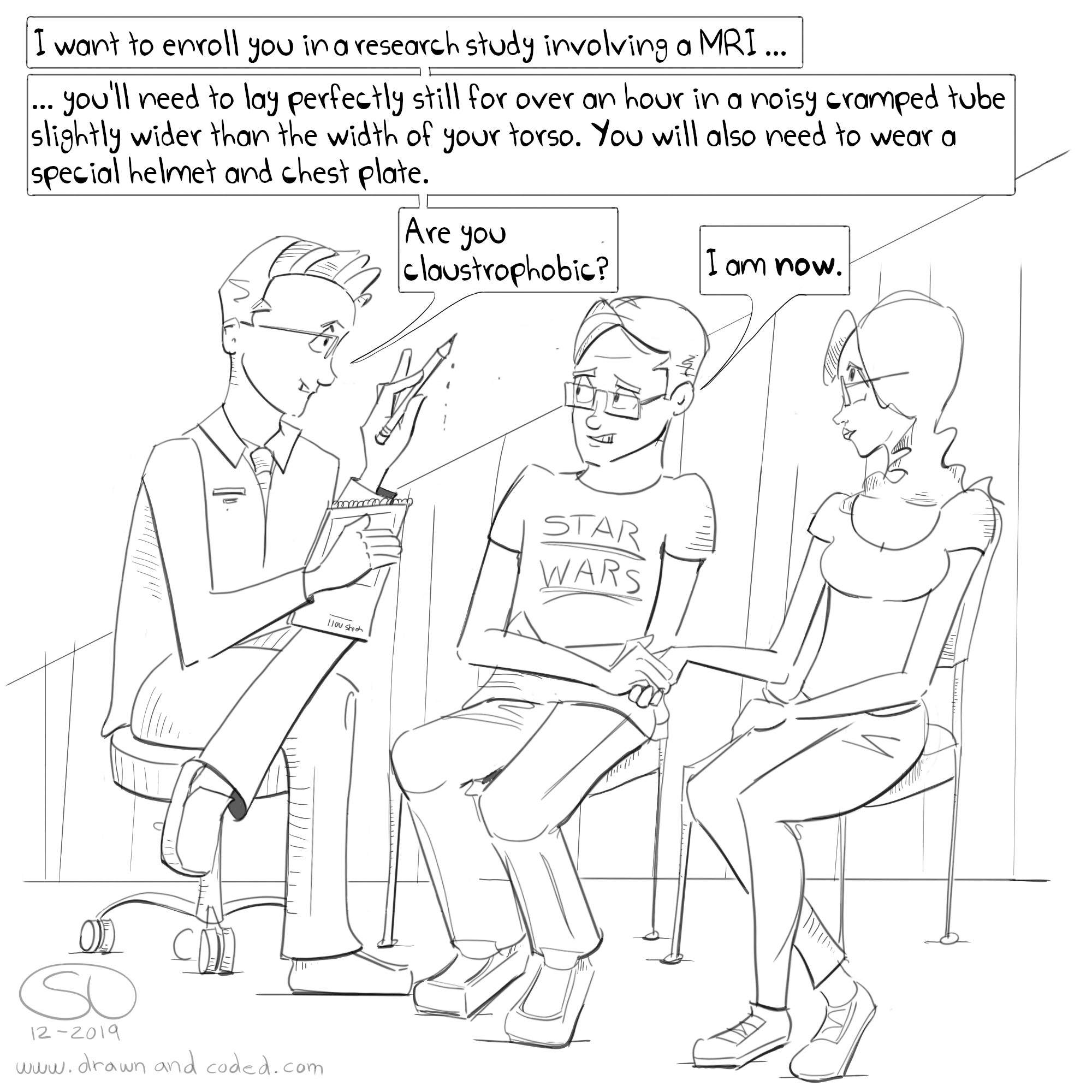
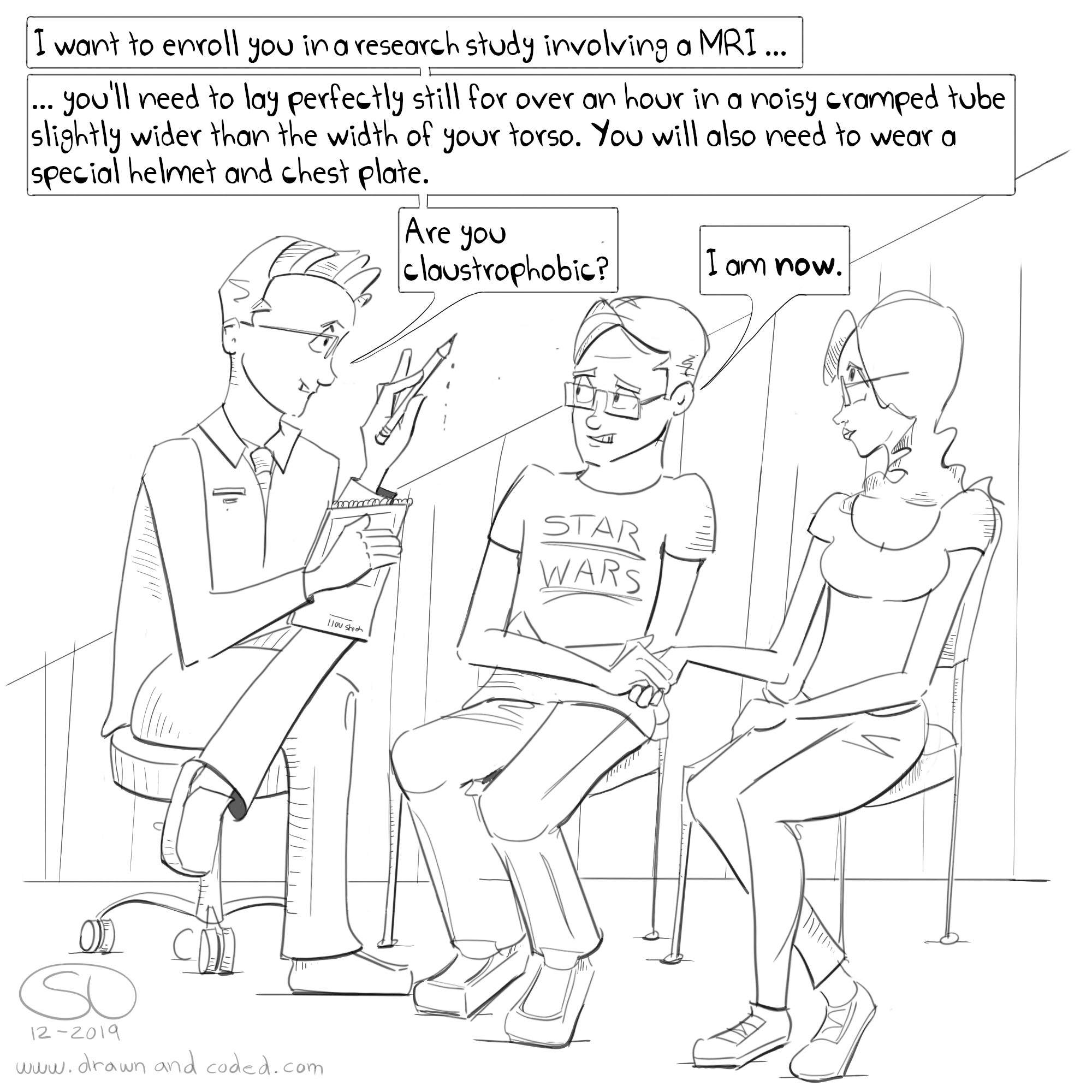
The big question when it comes to cancer – any cancer is if and where the cancer has spread. Localized cancer and metastasized cancer are treated very differently. As treatments are inevitably harsh on the patients’ body, a doctor wants to make sure that the treatment fits the disease. For me that meant more blood work, another CT Scan, this time of my chest, and an MRI Scan. Although I was also supposed to get either a PSMA or Axumin Scan done as well, availability and insurance approval has pushed those out to a later date.
I covered the blood work as well as CT Scans in prior posts so I’ll skip the details. MRI Scans, however, are uncharted territory and deserve some attention.
Dr. Stewart wanted an MRI Scan performed on my groin to get a better look at my prostate and nearby lymph nodes. I asked him what was wrong with the CT Scan that I had performed just a few weeks prior and was told that an MRI Scan produces more detailed images. MRI stands for “Magnetic resonance imaging”. An MRI uses a strong magnetic field to manipulate the atoms in your body. Radio waves are then used to create an image of the excited atoms. Fortunately, MRI Scans do not use radiation so they are relatively safe.
Another interesting factoid : Chemotherapy and recent tattoos (within 30 days) are a no-no for MRI. While talking to the MRI receptionist I found out that the electromagnets heat up the ink and/or chemicals. Naturally, pacemakers and any metal objects make you ineligible as well. I’m so glad I didn’t get that tattoo on my ass that says, “F*ck Cancer”.
Prior to my procedure the MRI technician guided me to the bathroom and in broken English advised me that, “Clean balls will help the machine produce a better image.” She then turned and walked away leaving my wife and I to ponder the logistics of such a task given that the bathroom had no shower. We eventually decided that the technician actually said “clean bowels”. After complying I met the technician in the MRI room.

You literally lie perfectly still in a long narrow tube for about an hour with your nose mere inches from the ceiling. It would be peaceful if it weren’t for the constant loud hum and banging of the machine’s electromagnets toggling on and off.

Let’s take a step back for a moment to tally up everything. So far I’ve had :
2 CT Scans.
1 MRI.
4 PSA Tests.
2 Ultrasounds.
1 Genetic screening of my blood and biopsy.
1 Bacterial analysis of my semen.
1 Prostate Biopsy.
3 Digital Rectal Exams (DRE).
8 Prescriptions; 4 of which were for Antibiotics
30 Appointments with Doctors and Therapists.
That is a lot of information for an organ that started off the size of a walnut. Given all that information I’ve realized one important thing and that is :
For prostate cancer, and I assume any type of chronic disease you will likely want to consult with doctors across different networks. Every single one of those doctors will want to see these records. The problem is hospitals are terrible at sharing. This is done to protect you, the patient. HIPPA, or “Health Insurance Portability and Accountability” Act of 2003 made the process a lot easier but 16 years later, hospitals are still struggling to upgrade their systems to adhere to the new regulations. Record transfers between networks typically require a faxed ( yes, fax ) request.
In software development we have a term called “Sneaker Net”. Prior to the internet and networked computers the only way to copy a file from one computer to another was to put the file on a disk and physically walk the disk between the computers. Although hospitals are digitizing their records, they are doing it at a glacial pace. While some records can be emailed, images produced by scans must be copied to a CD. This CD must then be walked, or “Sneaker Net”’ to the requesting hospital. I spent two hours on Wednesday doing exactly this to get my original CT and Bone Scans from Scripps to UCSD.
Following the dismissal of the board I met with Dr. Stewart to go over the treatment options they had discussed. My mom and my wife, Jodie joined me in an hour-and-a-half discussion.
First the good news. The CT Scan of my chest came back clear. There was no evidence of the cancer metastasizing there. In addition, the MRI scan showed my prostate and enlarged lymph node pretty much unchanged since my first CT scan from a few weeks ago.
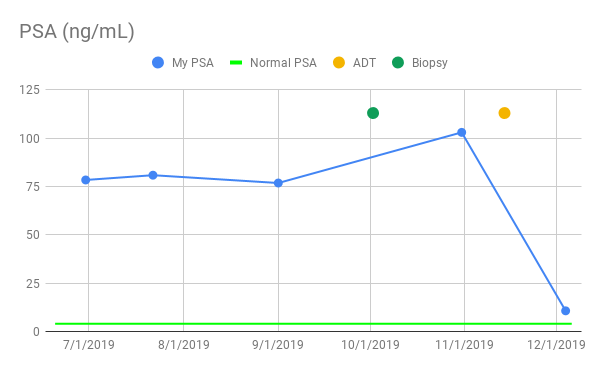
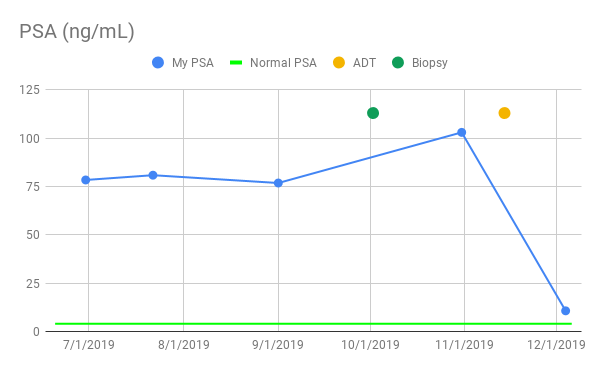
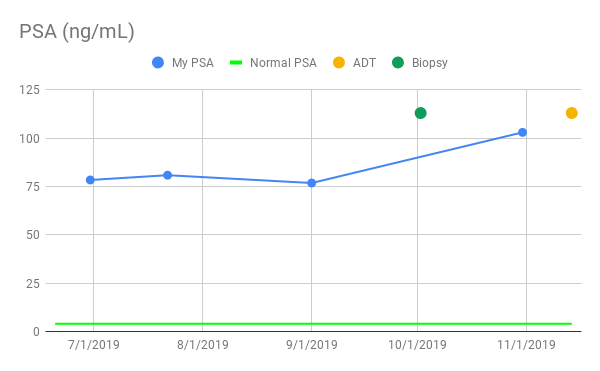
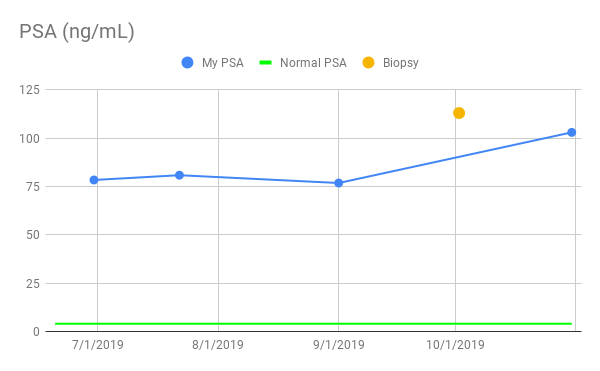
Now the not so good news. My prostate and lymph node were still teeming with prostate cancer. Furthermore, my blood test indicated that my PSA was climbing. Prior to my biopsy it had been in the high 70’s. Now it was 103. Dr. Stewart told me that due to my young age, the aggressiveness of my cancer, and my high PSA that my situation did not fit the typical treatment protocol. He wanted to think “outside of the box” and be very aggressive with my treatment. In short, the “Tumor Board” couldn’t make a unanimous decision. Instead, they came up with three treatment options :
You’ll notice that the only commonality between all three treatments is hormone therapy. Hormone therapy is used in conjunction with radiation, chemotherapy, and surgery. It’s complementary and doesn’t affect the administering of the other treatments. As such it was the main topic of discussion for our meeting and the first treatment that Dr. Stewart wanted to administer.
As I mentioned in a prior post, testosterone feeds prostate cancer. By doing away with testosterone you can starve the prostate cancer cells – at least for a while. Here’s the rub – hormone therapy doesn’t work forever. Eventually prostate cancer cells gain the ability to produce their own testosterone, or are no longer dependent on it. Hormone therapy is also known as “androgen deprivation therapy, or ADT.
In fact, the alternative to hormone therapy is the removal of the tesicles which is known as an “orchiectomy”. Fortunately, this is seldom done anymore but that didn’t stop Jodie and I from joking about the potential upside of prosthetics.
“Would you go larger, say the male equivalent of a DD bra?”, I joked.
“Or, would you go smaller to make everything else look larger?”, Jodie retorted.
Fortunately, Dr. Stewart and my mom had a good sense of humor throughout this discussion.
Now for the side effects. They include fatigue, muscle loss, weight gain, osteoporosis, libido, mood swings, breast tenderness, and hot flashes. I joked with Jodie that if I could of delayed my cancer for another 15 years that we could of gone through menopause together.
Yeah, so the side effects suck. It sounds like weight lifting as well as increasing my vitamin intake will help. Given that the treatment is to be administered over two years well, it’s going to be a long two years.
Lupron is the most common medication administered for ADT. It is administered as a shot every three months. However, given that my PSA is rising Dr. Stewart decided to put me on a different medication called Degarelix, also known as (ahem) Firmagon. Dr. Stewart chuckled at this and we caught on immediately.
“You’ve got to be kidding me. Who names a drug that saps your testosterone FIRMagon?”, I asked. “Someone in marketing has a sick sense of humor.”
Dr. Stewart didn’t really have much of an answer but explained that Flacidagon, unlike Lupron does not cause your testosterone levels to temporarily spike and would have a better chance of keeping my cancer in check.
It was then that Dr. Stewart told us that testosterone, in addition to being produced by the testicles is also produced by the adrenal glands. As such he also wanted to prescribe me another medication called Zytiga. Up until this point I had not asked about the cost of all of the medications but Zytiga rang a bell. I vaguely remembered coming across it while browsing the web.
“Um. So, how much does Zytiga cost?”, I asked.
When Dr. Stewart deflected by talking about insurance approval and financial assistance I knew that I had struck a chord. He eventually told me that if I had to pay more than $50 per month that I could probably work something out with financial assistance. Naturally my curiosity got the better of me. After our appointment I consulted Google and realized that Zytiga costs ( ready for this? ) roughly $10,000 per month.
Ouch.
Zytiga, in addition to draining the pocketbook can also affect your heart and liver. Dr. Stewart told me that while I was taking it I would need to have frequent blood screenings and monitor my blood pressure daily.
Even though there has been no evidence thus far of my cancer metastasizing outside my pelvic region I get the feeling that Dr. Stuart nor the “Tumor Board” are convinced. The deciding factor I believe, rests on the outcome of my pending PSMA or Axumin Scan. What’s the holdup? Well, the PSMA machine can only be performed at UCLA and is booked up for over a month. And then of course, there’s the approval required by my insurance company.
Cancer treatments are expensive. Because of this, I’ve realized that every medication and procedure needs explicit approval from my insurance company. Unfortunately, the approval process takes roughly three days. If an approval is requested on say, a three day weekend you’re looking at a significantly longer delay. When dealing with cancer there is a sense of unnerving urgency, too, like you’re half expecting an alien to burst through your stomach if you delay too long.
As soon as she realized that insurance was holding up my treatment she was on the phone with them. She doesn’t take no for an answer, either. Hopefully early next week I will get my first injection of hormone therapy and I will finally begin the initial stage of my treatment.
Take care. Stay healthy. Live life.
-Scott
Previous : Building My Team
Next : Drug Interactions

#prostatecancer #cancer #prostatitis #psa #prostate #urology #oncology #drawnandcoded #iwillbeatthis

Yesterday, while most of LA was trying to escape a fire that had broken out along the 405 near the Getty Museum my wife, Jodie and I raced towards it. I had an appointment with Dr. Stuart Holden, a urological oncologist at UCLA that had been recommended to me by a family friend.
I can best describe the UCLA Medicine complex as what would happen if a hospital building devoured several other hospital buildings and then plopped itself down in the middle of a bustling downtown. The size was bewildering! While checking in at Urology Jodie noticed that all of the doctors’ cards were arranged on a turnstile like the ones grocery stores use to display gift cards. We counted over 30 before finding and pocketing Dr. Holdens.
Last week I talked to Dr. Carrie Costantini, an oncologist at Scripps. She gave me two options, either remove my prostate, or bombard it with radiation. Dr. Holden told me that performing surgery was premature without first determining if the cancer had spread. He said that the treatment varies considerably depending on whether or not the cancer is contained within the prostate or has spread elsewhere. Furthermore, performing surgery or treatment before getting a full picture might make me ineligible for clinical trials.
These tests include a bleeding edge scan called a Ga-PSMA PET CT Scan. What a mouthful, right? In my last post I wrote about the Prostate-specific antigen ( PSA ) test for helping to detect prostate cancer. To clarify, PSA is a protein produced by the prostate. When the prostate is inflamed it produces more of it. Thus, it is commonly used as an indicator of cancer. As it turns out once prostate cancer has metastasized the PSA protein is not as accurate, particularly with aggressive cancer such as yours truly has. The Prostate-specific membrane antigen ( PSMA ) is another protein that’s prevalent in metastasized prostate cancer cells. This new PSMA scan can pinpoint exactly where prostate cancer has metastasized so that targeted drugs can be delivered. Or, at least that’s what Dr. Holden is trying to sell me on. The truth is? I believe him. The downside is that the test costs just shy of $3000, is not ( yet ) FDA approved, and I’ll have to drive UCLA to get it done. Hopefully the fires will have been extinguished by then.
Dr. Holden also wanted me to get a genetic screening done as he suspects my cancer is likely well, genetic. Whereas Scripps told me there was a 4 month lead time, Dr. Holden directed me to a company called Color Genomics. For $249 and some of your spit Color Genomics will determine if you have any known cancer genes including BRCA-1 and BRCA-2. BRCA stands for “BReast CAncer susceptibility gene”. Dr. Holden told me that my cancer treatment could vary based upon the findings produced by the genetic screening. Having the genetic screening performed will also help determine if my daughters might be at risk of cancer someday as well.
Lastly, Dr. Holden was perplexed why my initial CT Scan did not include my entire body. He told me that given my high PSA ( 78+ ) and Gleason ( 8-10 ) scores that it would be highly unlikely that the cancer would not have already metastasized. He told me that this warranted a CT Scan of my entire body – not just my groin area. He said that the CT Scan that I received was an impartial picture of the problem. Dr. Holden was just as perplexed why my prostate biopsy wasn’t guided by Magnetic Resonance Imaging ( MRI ). A urologist has the option of using an MRI machine to target specific regions of the prostate during a biopsy. My urologist removed 12 samples, or cores randomly from my prostate. In his defense however, he struck “gold” everywhere he dug.
Then Dr. Holden gave me yet another Digital Rectal Exam.
It’s just their way of saying, “Hi. Nice to meet you.” Fortunately, Dr. Holden admitted to having small hands before niceties were exchanged.
So what’s next? This Friday I have another second ( third? ) opinion with a Dr. Tyler Stewart a urological oncologist at UCSD’s Moores Cancer Society. After that I’ll have more than enough information to make an educated decision on what to do next.
Not for the last time I am incredibly grateful for the outpouring of support from everyone as I work through all of this. I can’t thank you enough. I’m beginning to realize that cancer is a full-time job but at the same time it’s important not to lose sight of what is important. I love you all. Take care. Eat Healthy. Stay Healthy.
Take care. Stay healthy. Live life.
-Scott
Previous : Prostate Cancer
Next : Building My Team

#prostatecancer #cancer #prostatitis #psa #prostate #urology #oncology #drawnandcoded #iwillbeatthis

After over 20 appointments with a variety of doctors and therapists it turns out my Prostatitis is in fact Prostate Cancer.
Back in May I started having some urinary issues. I was getting up several times a night to pee. I was having trouble starting and stopping. After I started peeing every half-hour I visited Urgent Care. The Urgent Care doctor diagnosed me with Prostatitis, a painful inflammation of the Prostate gland. A follow-up with two different urologists confirmed the diagnosis. Each urologist performed their own Digital Rectal Exam ( DRE ) and independently reported that I was sporting a “large squishy prostate with no noticeable tumors”. Sexy, right? My second urologist even went as far as to ( cough, cough ) “milk” my Prostate for bacterial analysis.
Due to my age ( 43 ) and the negative DRE’s I was put through several rounds of antibiotics and physical therapy. I was given a Prostate-specific antigen ( PSA ) test to see if I was a candidate for a drug called Finasteride. Finasteride is one of several drugs that is used to shrink the prostate. It is given to men with enlarged prostates, or Benign Prostatic Hyperplasia ( BPH ) to help alleviate symptoms. A PSA test is a simple blood test that is typically performed on men over 50 to check for prostate inflammation. PSA tests are not usually administered to men suffering from Prostatitis as the inflammation can skew the numbers. A PSA under 2.5 is considered normal. Mine? 78.38. I’ve always been an overachiever.
After two more elevated PSA tests ( 80.85 and 76.81 ) and persistent pain my urologist decided that I should get a Prostate Biopsy. A Prostate Biopsy is a surgical procedure where a doctor goes through your rear end ( yes, again ) and take 6-12 “cores”, or samples from the prostate. A pathology report is then performed and a Gleason Score is attributed with each sample. The Gleason Score measures the aggressiveness of the cancer. All 12 of my samples came back with cancer. 11 of the 12 were in the 8’s and 9’s. The 12th came back as a 10. My urologist, wife, and I were all shocked.
After a biopsy comes back positive for cancer the next thing a doctor does is prescribe scans to see if and where the cancer has spread. I spent the better part of a day with my wife, Jodie getting a Nuclear Bone Scan and a Computed Tomography ( CT ) Scan. A Nuclear Bone Scan is used to determine if the cancer has spread to your bones. It requires you to be injected with a small amount of radioactive material. After a couple of hours the material binds with the bones in your skeleton after which you are placed under a large machine resembling an automotive lift. The machine slowly moves down your body and detects where the radioactive material accumulated in your skeleton. A CT scan requires the injection of a “contrast” into your blood. This time you are placed in a large machine resembling an enormous toilet bowl. The machine takes a 3D image of your body and using the contrast, can determine if the cancer has spread to any nearby organs. After a radiologist reviews your scans you meet with an oncologist and for me, a surgeon.
Over the last couple of days I met with a surgeon and an oncologist to go over my scans. The good news is that my cancer hasn’t spread to my bones or any distant organs. The bad news is that it has likely spread to a nearby lymph node. The oncologist that I met with couldn’t accurately stage me through the biopsy or scans but predicted that I would be a “high” Stage III or a Stage IV. The big differentiation is that a Stage III is curable whereas a Stage IV is treatable.
The plan is to perform a Radical Prostatectomy, or the removal of my prostate and nearby lymph nodes on November 7th. The sole coolness factor is that the procedure is done robotically through two small incisions. The downsides are many. The recovery can take several months during which I will likely have incontinence, swelling, and libido issues. I imagine these are the some of the same issues a woman suffers after a C-Section without the benefit of a new baby at the end. Three months following my surgery another PSA test will be administered. If everything goes well my PSA test will be zero and I will just have to have regular tests administered to track any signs of cancer. However, if my PSA test is not zero it means that my cancer still persists and I will likely undergo radiation and hormone suppressing treatment. For good measure I am planning on getting two more second opinions from other oncologists prior to my surgery.
As of yesterday, my daughters, Ashley and Kaylee are aware of my Prostate Cancer. Their first question was obviously, “Are you going to die?”. I caught myself before responding, “…well, everyone does at some point” and told them firmly, “No. Absolutely not.” After a few more questions they happily went about their evening and promptly went across the street to the neighbors house to disseminate the news. At bedtime I read them a book my mom bought me called, “Cancer Party”. I can’t recommend this book enough for younger children. It takes a lighthearted informative approach to explaining everything cancer, radiation, and chemotherapy.
In the meantime my wife, Jodie has taken it upon herself to help cure me through food. She’s read more books on healthy eating over the past few months than I can count. Together we have become superfood-eating pescatarians because God forbid we give up sushi. Our Frappuccinos have been replaced with green tea and our ice cream with dark chocolate. It would be a lot more traumatic if she weren’t such a good cook.
Moving forward I plan on posting regular updates on my progress here at DrawnAndCoded. I never ever intended this site to be used in such a manner but I am uncomfortable posting on normal social media channels such as Facebook. My ultimate goal will be to keep everything as upbeat and informative as possible. And yes, there will still be comics and the occasional programming article as well.
Last but not least. Since my Prostate Cancer diagnoses I have received an overwhelming amount of support from my family, my friends, and complete strangers ( now, friends ). You know who you are. Thank you for your love and support. And please keep it coming.
Take care. Stay healthy. Live life.
– Scott
Previous : Physical Therapy
Next : A Second Opinion
#prostatecancer #cancer #prostatitis #psa #prostate #urology #oncology #drawnandcoded #iwillbeatthis
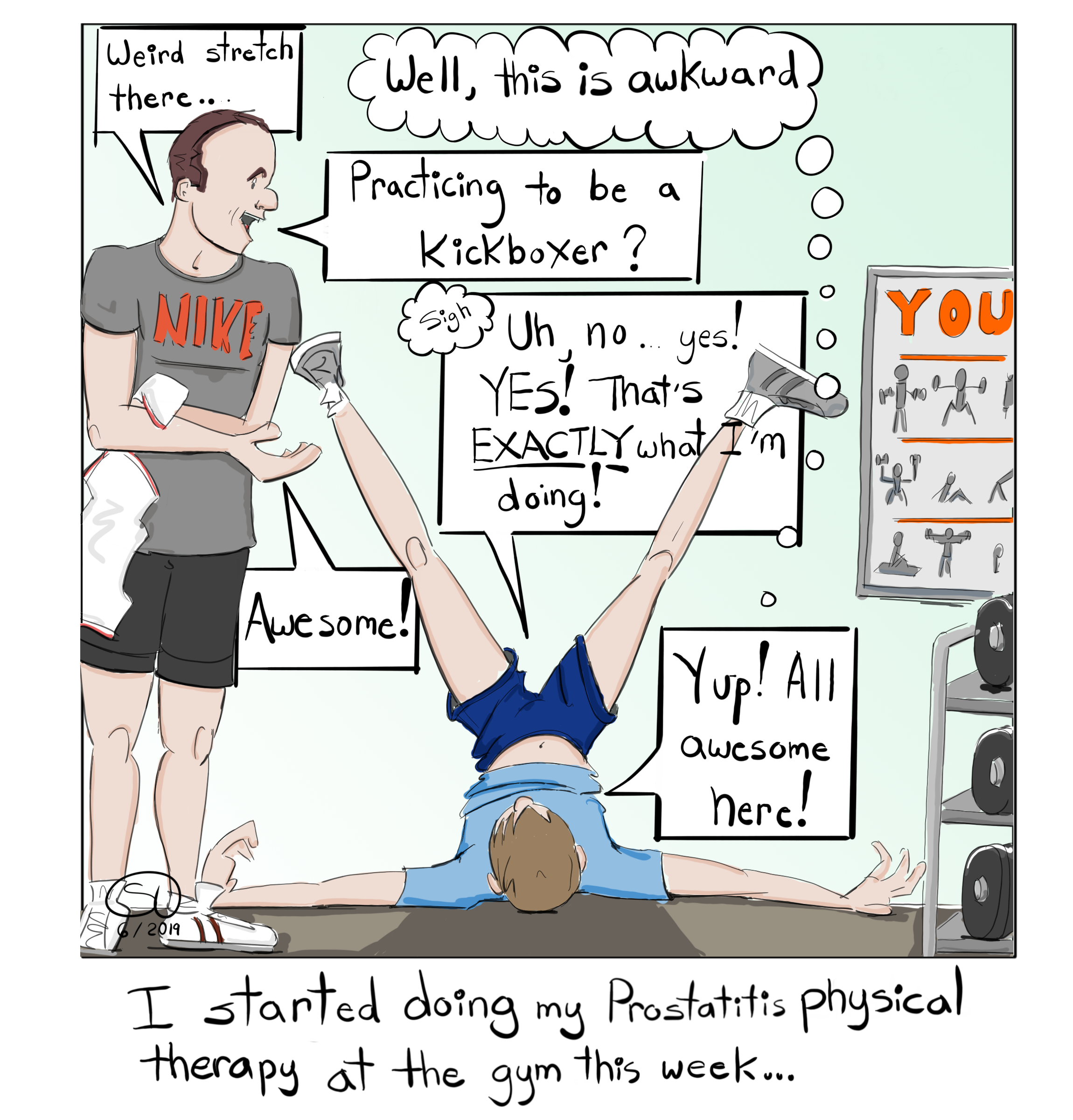
My urologist prescribed me physical therapy to help treat my Prostatitis symptoms. Thank you Jodi Tam of Renew Physical Therapy for making the pain so much more tolerable. The stretches you have prescribed are incredibly effective – if not socially awkward….
Take care. Stay healthy. Live life.
– Scott
Previous : Prostatitis
Next : Prostate Cancer
#prostatitis #prostate #chronicpelvicpainsyndrome #cpps #Ciprofloxacin #Doxycycline #bactrim #tamsulosin #chronicpain #yoga #physicaltherapy #stretching #drawnandcoded #comic